History
The patient is a 28 yo man referred on a walk-in basis with an eight month history of a bullous eruption on the dorsum of his left hand. He gets one or two painless lesions a month. No history was sent over with the patient and he is a poor historian. His medications include Welbutrin, Clozeril and Soma (carisprodol/aspirin)
Exam:
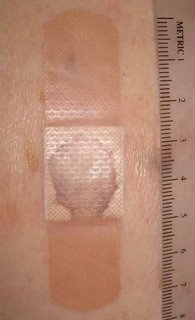
The only findings are on the dorsum of the left hand. Here, there is a hemorrhagic bulla, a vesicle and areas of mild erythema at sites of previous lesions.


Biopsy:
I suspect fixed drug or pseudoporphyria cutanea tarda. I biopsied the small papule and the edge of the bullae and made a follow-up appointment.
Path Report:
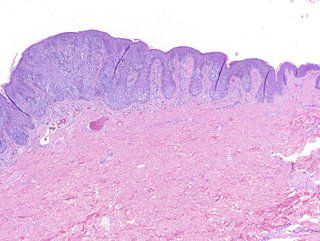
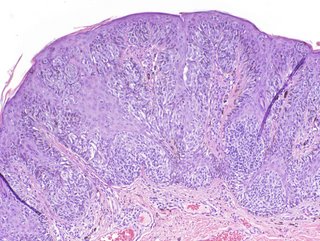
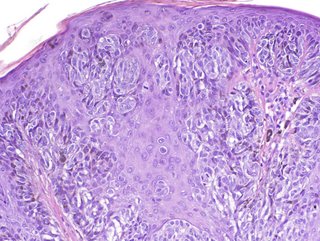
A subepidermal separation, individually necrotic keratinocytes , and a sparse superficial perivascular lymphocytic infiltrate with occasional neutrophils .
NOTE : (A and B). Amphophilic globular material is seen deposited in the dermis and around blood vessels in both specimens. This material is P.A.S. stain positive, and stains negative for amyloid and elastic tissue. The differential diagnosis could include porphyria cutanea tarda , although this is usually less inflammatory. A subepidermal autoimmune bullous disorder could also be considered. An additional biopsy for direct immunofluorescence may be of help.
Laboratory Studiess:
CBC normal, LFTs normal, ferritin normal. Hep B and C negative, All urinary porphyrins well within normal levels. Uroporphyrin: 9.6 ug (nl < 30.0) Coproporphyrin 40 ug (normal < 65/24 hr)
Discussion: This is likely pseudoporphyria cutanea tarda. A similar case has been reported. Your comments are welcomed.

The patient is a 28 yo man referred on a walk-in basis with an eight month history of a bullous eruption on the dorsum of his left hand. He gets one or two painless lesions a month. No history was sent over with the patient and he is a poor historian. His medications include Welbutrin, Clozeril and Soma (carisprodol/aspirin)
Exam:
The only findings are on the dorsum of the left hand. Here, there is a hemorrhagic bulla, a vesicle and areas of mild erythema at sites of previous lesions.


Biopsy:
I suspect fixed drug or pseudoporphyria cutanea tarda. I biopsied the small papule and the edge of the bullae and made a follow-up appointment.
Path Report:
A subepidermal separation, individually necrotic keratinocytes , and a sparse superficial perivascular lymphocytic infiltrate with occasional neutrophils .
NOTE : (A and B). Amphophilic globular material is seen deposited in the dermis and around blood vessels in both specimens. This material is P.A.S. stain positive, and stains negative for amyloid and elastic tissue. The differential diagnosis could include porphyria cutanea tarda , although this is usually less inflammatory. A subepidermal autoimmune bullous disorder could also be considered. An additional biopsy for direct immunofluorescence may be of help.
Laboratory Studiess:
CBC normal, LFTs normal, ferritin normal. Hep B and C negative, All urinary porphyrins well within normal levels. Uroporphyrin: 9.6 ug (nl < 30.0) Coproporphyrin 40 ug (normal < 65/24 hr)
Discussion: This is likely pseudoporphyria cutanea tarda. A similar case has been reported. Your comments are welcomed.