Abstract: 6 yo boy with one month history of an eschar on the neck
History: This six year old boy has had an indurated nodule on the left posterior nuchal area for around a month. He is a high functioning patient on the autism spectrum. No history of antecedent trauma or envenomation is available. He is well otherwise with no complaints of constitutional symptoms or headache.
O/E: 1 cm escharotic lesion left posterior neck. Surrounding area is indurated. No other cutaneous findings.
Clinical Photo:
 |
| photo courtesy of Yoon Cohen, D.O. |
Labs: A wound culture was obtained.
The eschar was sharply dissected. We attempted to anesthetize the area for an incisional biopsy but patient was not compliant.
Discussion: The patient lives in an endemic area for Lyme disease. There are many ticks in the environment. The wound may represent a reaction to a tick bite. The differential diagnosis in patients with similar eschars includes rickettsial infections, cutaneous anthrax, tularaemia, necrotic arachnidism (brown recluse spider bite), scrub typhus (Orientia tsutsugamushi), rat bite fever (Spirillum minus), staphylococcal or streptococcal ecthyma, and Lyme disease.
Diagnosis: Considering where this patient lives, the most likely diagnosis is tick bite reaction.
References:1. Tick-borne lymphadenopathy (TIBOLA) acquired in Southwestern Germany Free Full Text Siegbert Rieg1 et. al siegbert.rieg@uniklinik-freiburg.de
BMC Infectious Diseases 2011, 11:167 doi:10.1186/1471-2334-11-1672. African tick-bite fever: a new entity in the differential diagnosis of multiple eschars in travelers. Description of five cases imported from South Africa to Switzerland. Althaus F, Greub G, Raoult D, Genton B. Int J Infect Dis. 2010 Sep;14 Suppl 3:e274-6. doi: 10.1016/j.ijid.2009.11.021. Epub 2010 Mar 15.
Abstract: African tick-bite fever (ATBF) is a newly described spotted fever rickettsiosis that frequently presents with multiple eschars in travelers returning from sub-Saharan Africa and, to a lesser extent, from the West Indies. It is caused by the bite of an infected Amblyomma tick, whose hunting habits explain the typical presence of multiple inoculation skin lesions and the occurrence of clustered cases. The etiological agent of ATBF is Rickettsia africae, an emerging tick-borne pathogenic bacterium. We describe herein a cluster of five cases of ATBF occurring in Swiss travelers returning from South Africa. The co-incidental infections in these five patients and the presence of multiple inoculation eschars, two features pathognomonic of this rickettsial disease, suggested the diagnosis of ATBF. Indeed, the presence of at least one inoculation eschar is observed in 53-100% of cases and multiple eschars in 21-54%. Two patients presented regional lymphadenitis and one a mild local lymphangitis. Though a cutaneous rash is described in 15-46% of cases, no rash was observed in our series. ATBF was confirmed by serology. Thus, ATBF has recently emerged as one of the most important causes of flu-like illness in travelers returning from Southern Africa. The presence of one or multiple eschars of inoculation is an important clinical clue to the diagnosis. It can be confirmed by serology or by PCR of a biopsy of the eschar. Culture can also be done in reference laboratories. Dermatologists and primary care physicians should know this clinical entity, since an inexpensive and efficient treatment is available.3. Histologic features and immunodetection of African tick-bite fever eschar.
Free Full Text Lepidi H, Fournier PE, Raoult D. Emerg Infect Dis. 2006 Sep;12(9):1332-7.
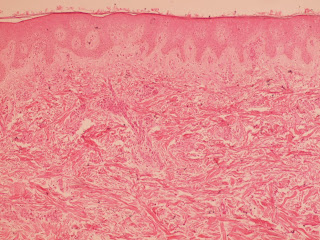
African tick-bite fever (ATBF) is a rickettsiosis caused by Rickettsia africae. We describe histologic features and immunodetection of R. africae in cutaneous inoculation eschars from 8 patients with ATBF, which was diagnosed by culture or association of positive PCR detection and positive serologic results. We used quantitative image analysis to compare the pattern of inflammation of these eschars with those from Mediterranean spotted fever. We evaluated the diagnostic value of immunohistochemical techniques by using a monoclonal antibody to R. africae. ATBF eschars were histologically characterized by inflammation of vessels composed mainly of significantly more polymorphonuclear leukocytes than are found in cases of Mediterranean spotted fever (p < 0.05). Small amounts R. africae antigens were demonstrated by immunohistochemical examination in 6 of 8 patients with ATBF. Neutrophils in ATBF are a notable component of the host reaction, perhaps because ATBF is a milder disease than the other rickettsioses. Immunohistochemical detection of rickettsial antigens may be useful in diagnosing ATBF.
4.
The Expanding Spectrum of Eschar-Associated Rickettsioses in the United States Free Full Text W. Chad Cragun, MD; Brenda L. Bartlett, MD; Michael W. Ellis, MD; Aaron Z. Hoover, MD; Stephen K. Tyring, MD, PhD, MBA; Natalia Mendoza, MD; Todd J. Vento, MD, MPH; William L. Nicholson, PhD, MS; Marina E. Eremeeva, MD, PhD; Juan P. Olano, MD; Ronald P. Rapini, MD; Christopher D. Paddock, MD, MPHTM
Arch Dermatol. 2010;146(6):641-648. doi:10.1001/archdermatol.2010.48.
.