Abstract: 83 yo man with a mixed desmoplastic melanoma of the scalp
HPI: In August 2013, this 83 yo man was seen with an 8 mm diameter nodule on the left parietal scalp present for 4 – 5 months and growing rapidly. He had a history of two thin melanomas excised from the left forhead and left temple from 2009 – 2011. In reviewing the biopsy reports, it can not be determined if they were both the same lesion or two separate tumors.
O/E: 8 mm pink to red well-circumscribed nodule left parietal. The dermatoscopic image shows multiple polymorphous blood vessels with central crystalline structures and a pink hue (vascular blush ) in the background. No palpably enlarged lymph nodes.
Clinical Photos:
 |
| Dermoscopic Image - Courtesy of Yoon Cohen |
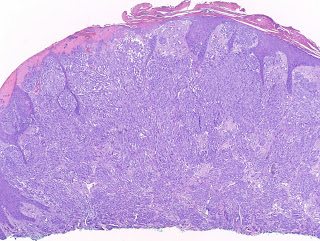
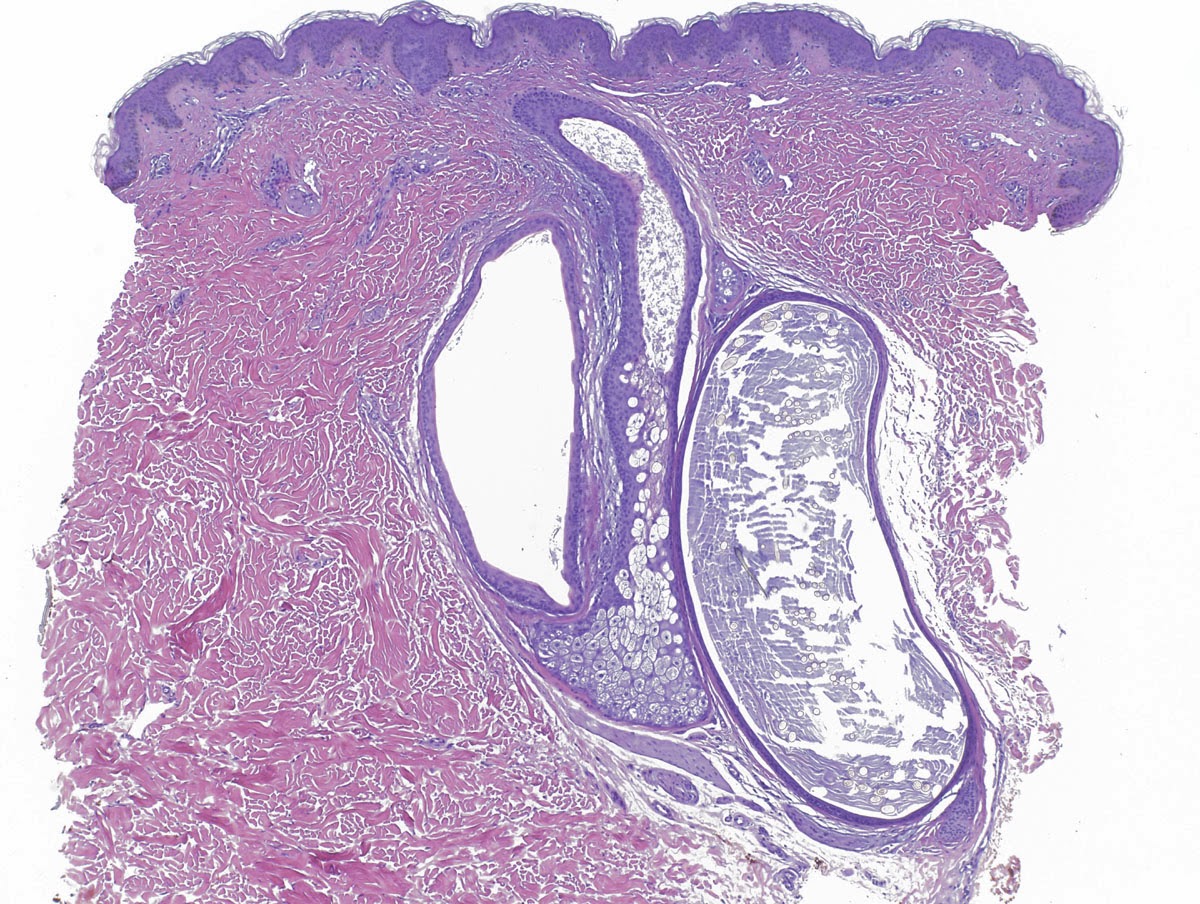
Pathology: Desmoplastic melanoma > 7.35 mm thick. Level 5. The tumor was/was not purely desmoplastic but over 10% of the cells has a spindle and epitheloid component as well.
Lab and Xray:
All blood studies including LDH within normal range.
P.E.T. Scan no abnormal foindings
Surgical Treatment: Patient underwent a WLE with 2 cm margins on October 2, 2013. The defect was closed with a fasciocutaneous flap. Sentinel lymphnode biopsy was not performed.
Diagnosis: Desmoplastic melanoma with mixed histology, greater than 7.25 mm thick No evidence of distant spread.
The patient has been seen at two centers for discussion of further treatment. Local radiotherapy was recommended at both, although two different protocols were discussed. The patient is undecided if he wants radiotherapy at this time.
Discussion: The literature indicates that local radiotherapy reduces the incidence of local recurrence, but it is unclear if it provides an overall survival benefit. At least one study suggests that patients undergoing local radiotherapy have a lower survival (ref 1 below). It does not mention if these patients had more advanced disease that those who did not receive radiotherapy.
Questions: What would your recommendations to this patient be? Would you favor local radiotherapy? See Discussion above.
References:
1. Desmoplastic melanoma - the step-child in the melanoma family?
Wasif N, Gray RJ, Pockaj BA.
J Surg Oncol. 2011 Feb;103(2):158-62.
Abstract
BACKGROUND AND OBJECTIVES: Desmoplastic melanoma (DM) is a rare variant of cutaneous melanoma. Our goal was to study the surgical management of DM, identify prognostic factors, and impact of treatment options.
METHODS: Patients with DM (n = 1,735) were identified from the Surveillance, Epidemiology, and End Results database (1988-2006).
RESULTS: The median age of the study population was 69 years and overall survival (OS) at 5 years 65%. DM was more common in males (65%), most commonly found on the head and neck (51%), and had a mean thickness of 2.97 mm. Patients undergoing a wide local excision (WLE; ≥1 cm) had improved 5-year OS compared to a simple excision (<1 cm) or biopsy alone (67% vs. 60% vs. 45%, respectively, P < 0.001). Of 505 patients (29%) undergoing sentinel node biopsy (SLNB), only 14 (2.8%) were positive. Traditional prognostic factors such as Breslow thickness, nodal positivity, and ulceration did not predict survival. On multivariate analysis only adjuvant radiation therapy [HR 1.65 (95% CI 1.17-2.31)] and WLE correlated with survival [HR 0.47 (95% CI 0.32-0.69)].
CONCLUSIONS: Desmoplastic melanoma does not share traditional prognostic factors with the melanoma family. Surgical resection with wide margins is needed to optimize survival and routine SLNB may be unnecessary. Furthermore, patients who received adjuvant radiation were at increased risk of dying (HR 1.65) and had decreased OS at 5 years (66% no radiation vs. 50% for adjuvant radiation, P < 0.001). Importantly, none of the traditional prognostic factors for cutaneous melanoma, such as site, Breslow thickness, Clark level, ulceration, and nodal status, had any impact on survival on univariate or multivariate analysis. 2.
Mixed versus pure variants of desmoplastic melanoma: a genetic and immunohistochemical appraisal. Free Full TextMiller DD, Emley A, Yang S, Richards JE, Lee JE, Deng A, Hoang MP, Mahalingam M.
Abstract
Desmoplastic melanoma is subclassified into pure and mixed variants with a higher rate of lymph node metastasis in the latter. Given that reasons for these biological differences are not currently known, we investigated these subtypes with techniques that included genetic and immunohistochemical analyses of 43 cases of desmoplastic melanoma (24 pure, 19 mixed). Direct DNA sequencing was performed on BRAFV600E, RET gene (coding region on exon 11) and KIT (exons 11, 13 and 17). Immunohistochemical stains were performed with antibodies to markers of significance with respect to biological potential of nevomelanocytic proliferations and/or desmoplastic melanoma (Ki-67, CD117, nestin, clusterin, SOX10 and CD271/p75NTR). Polymorphism at the RET coding region (RETp) was noted in 33% of pure (8/24 cases) versus 24% of mixed (4/17 cases); BRAFV600E was absent in all cases of pure (0/24 cases) versus 6% of mixed (1/17 cases); no mutations were found in any of the cases on analyses of exons 11, 13 and 17 of the c-KIT gene (P=NS for all). For immunohistochemical analyses of pure versus mixed: mean percentage of Ki-67 nuclear positivity was 5% (s.d.=5.6) versus 28% (s.d.=12.6, P<0.001); CD117 stained 26% (6/23 cases) versus 78% (14/18 cases, P<0.01); nestin stained 83% (n=19/23 cases) versus 89% (16/18 cases, P=NS); clusterin stained 4% (1/23 cases) versus 6% (1/18 cases, P=NS); SOX10 87% (20/23 cases) versus 94% (17/18 cases, P=NS) and CD271 stained 61% (14/23 cases) versus 67% (12/18 cases, P=NS). Increased CD117 staining in the mixed variant suggests that alterations in the KIT protein may be involved in tumor progression. In addition, the proliferative index of the mixed variant was higher than that of the pure variant.
3.Subclassification of desmoplastic melanoma: pure and mixed variants have significantly different capacities for lymph node metastasis.
George E, McClain SE, Slingluff CL, Polissar NL, Patterson JW.
J Cutan Pathol. 2009 Apr;36(4):425-32.
Abstract
BACKGROUND: There is disagreement about the behavior and optimal management of desmoplastic melanoma (DM), particularly regarding the incidence of lymph node (LN) involvement. Recently, investigators have noted the frequently heterogeneous histologic composition of DM and have found significant differences between pure desmoplastic melanoma (PDM) (>or=90% comprised of histologically typical DM) and mixed desmoplastic melanoma (MDM) [>or=10% DM and >10% conventional melanoma (CM)].
METHOD: We reviewed 87 cases of DM comparing the histologic and clinical features of PDM (n = 44) to MDM (n = 43).
RESULTS: At surgical staging, there were LN metastases in 5 of 23 (22%) MDM patients, whereas all 17 PDM patients had negative LN biopsies (0%) (p = 0.04). PDM was less often clinically pigmented (36% vs. 67%) and had a lower mean mitotic index (1.3 vs. 3.0).
CONCLUSIONS: There are differences between PDM and MDM, the most important of which is the incidence of LN involvement. Our findings support the clinical utility of classifying DM into pure and mixed subtypes because the negligible rate of nodal involvement in PDM does not support the routine performance of sentinel LN biopsy in this subgroup of melanoma patients. In contrast, the incidence of LN involvement in MDM is comparable to that of CM.
4. Desmoplastic malignant melanoma: a systematic review.
Lens MB, Newton-Bishop JA, Boon AP. Br J Dermatol. 2005 Apr;152(4):673-8.
Abstract
Prompt definitive surgical excision is the treatment of choice for DM. Improved knowledge of the clinical behaviour and histological features of DM is important for more effective management of patients with DM.
5. Desmoplastic melanoma: a review.
Chen LL, Jaimes N, Barker CA, Busam KJ, Marghoob AA.
Abstract: Desmoplastic melanoma (DM) is a variant of spindle cell melanoma typically found on chronically sun-damaged skin of older individuals. Early diagnosis can be challenging because it is often amelanotic and has a predominantly dermal component. DM can be difficult to diagnose not only clinically but also histologically, and can be mistaken for a variety of benign and malignant nonmelanocytic spindle cell tumors when viewed on prepared histopathology slides. Pathologists have observed that DMs can manifest significant variation with respect to the extent of intratumoral cellularity, fibrosis, and/or perineural invasion. Furthermore, some tumors present with a pure desmoplastic invasive component (>90%) while other tumors display mixed features of DM and nondesmoplastic melanoma. This has led to the separation of DM into 2 histologic subtypes, pure and mixed. With a focus on the distinction between pure and mixed DM, this review will detail what is currently known about the diagnostic features of DM, discuss risk and prognostic factors, and examine the current literature on disease progression and management.





















.jpg)