The patient is a 49 yo man with a one month history of a very painful leg ulcer.
He is 8 years s/p heart transplant.
His medications include: CsA, CellCept, Pred, Diltiazem, Ranitidine.
There was no history of trauma and no similar ulcers in the past. He works at a supermarket and is on his feet all day long at work.
This ulcer is periodically painful. He has had leg edema for over a year.
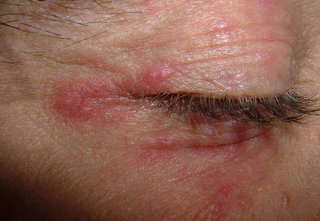
The examination shows an 8 mm in diameter ulcer with as slightly purulent surface and ragged edges.. The borders are grayish. The area surrounding the ulcer has 2+ pitting edema and is erythematous.

Bacterial culture shows only staph species
Peripheral pulses are present but weak.
No response to support stocking used for the past three weeks.
This is probably a venous ulcer, but it's a bit unusual for a 49 yo man. Diltiazem can cause edema.
The pain is out of proportion to what one would expect. I have known the patient for six years and he has not had pain like this before.
Please help with diagnostic and therapeutic suggestions.
He is 8 years s/p heart transplant.
His medications include: CsA, CellCept, Pred, Diltiazem, Ranitidine.
There was no history of trauma and no similar ulcers in the past. He works at a supermarket and is on his feet all day long at work.
This ulcer is periodically painful. He has had leg edema for over a year.
The examination shows an 8 mm in diameter ulcer with as slightly purulent surface and ragged edges.. The borders are grayish. The area surrounding the ulcer has 2+ pitting edema and is erythematous.

Bacterial culture shows only staph species
Peripheral pulses are present but weak.
No response to support stocking used for the past three weeks.
This is probably a venous ulcer, but it's a bit unusual for a 49 yo man. Diltiazem can cause edema.
The pain is out of proportion to what one would expect. I have known the patient for six years and he has not had pain like this before.
Please help with diagnostic and therapeutic suggestions.